The following posts are based on updates I created on CaringBridge during Steve’s stay, providing a narrative of love and survival in its rawest form.
March 28th, 2024, was a Thursday like any other—until it wasn’t. On that day, our world was upended in an instant. My beloved soulmate, Steve, decided to go for a bike ride at around 3 p.m. Usually, he ventures out first thing in the morning, but for some reason, he felt a compelling urge to ride later that day. It was a beautiful spring day in Arizona, the kind that coaxes you outdoors with its warm breeze yet isn’t too hot. Steve set off to survey the neighborhood, not knowing he was embarking on a journey none of us expected.
Meanwhile, I was in my office, engrossed in crafting a travel itinerary for a friend’s upcoming trip to Spain. My mind was lost in the vibrant streets of Barcelona, dreaming of luxury hotels and cultural excursions. Steve returned from his ride and deviated from the daily ritual of plopping down in his chair near my desk to provide me with a detailed report on the neighborhood happenings. At the time, I barely registered the break in pattern.
Five minutes later, he called for me, his voice tinged with panic—something was terribly wrong. I spun around in my chair and rushed to the living room. The calm spring day shattered as Barcelona was left on the sleeping screen, forgotten.
“I need to go to the hospital,” he gasped. I found him disoriented and sweating in the living room. The symptoms—cold sweats, indigestion-like pain, a tingling arm, escalating to chest pain—unfolded within moments, a rapid progression that left no time for Google searches or second guesses. Everything happened in a surreal blur of slow-motion chaos and lightning-fast terror.
“Everything happened in a surreal blur of slow-motion chaos and lightning-fast terror.” ~ Tracy Jo
Moments later, Steve collapsed onto the couch, and his heart stopped. I was already on the phone with 911. From somewhere deep inside him, a long continuous snore reverberated through our quiet home as I frantically pleaded for help, “My husband is having a heart attack and is dying. Please hurry.”
I jumped onto his lap and gently patted his cheeks as his eyes grew distant. I didn’t realize his heart had stopped because his eyes were wide open, although they were unfocused and vacant. His face took on a purplish hue, and blood vessels began spreading like a travel map across his nose and cheeks. A deep, guttural snore—the haunting sound of life slipping away—echoed through the room. That sound, and the vacant stare in his eyes, are etched into my memory, haunting reminders of the fragility of life.
The dispatcher remained calm and asked if Steve was lying flat. “No,” I exclaimed, “he’s sitting on the couch.” I was instructed to quickly move him to a flat, solid surface. I put the phone on speaker mode, and fueled by adrenaline, grabbed Steve’s ankles, and in one swift pull, launched him from the couch to the floor with a force that shocked even me.
With no time to spare, I focused on the dispatcher’s steady voice as he guided me through the steps to begin chest compressions—a rhythmic pumping of the heart as I sang “Stayin’ Alive” and counted out loud so the dispatcher could advise me to speed up or slow down. “Keep your elbows locked,” he instructed. I’d taken a class years ago, but the process is different now—just compressions. I remembered where to place my hands, to push hard enough to crack ribs, and the song “Stayin’ Alive.”
“Stayin’ Alive”, both a literal anthem and a guide for CPR, became my desperate chant as I worked to revive my husband. Each compression was a battle against time. Steve’s occasional gasps of air were false signs of recovery, just the rhythm of life being manually pumped back into him. In a surreal twist, a flash of menopausal inferno heat washed over me, but the urgency of the moment left no room for personal discomfort. There was no time to shed the sweatshirt that had transformed into an electric blanket on steroids.
“Stay with me, baby, stay away from the light,” I urged, clinging to hope as I listened for the approaching sirens.
I administered CPR for what seemed like hours but was actually only about six minutes. Every few minutes, Steve would gasp, and I thought he was breathing, but it was just the compressions working. “Stayin’ Alive, ah, ah, ah, ah,” I yelled at Steve, “Stay with me, baby, stay away from the light.”
My youngest son, Grady, is studying to be a firefighter, and in desperate need to give Steve something to hold on to, I kept saying, “I can hear the sirens. Grady’s coming, love…Stay with me. Don’t leave me.”
The 911 operator gave me a minute-by-minute countdown until the EMTs would arrive. It took the incredible Surprise Fire Department, Station 301, less than six minutes to walk through the front door. They took over immediately, continuing compressions and defibrillating him numerous times. They couldn’t get an IV line in, so they used an IV gun to insert a line directly into the bone marrow of his shoulder. He was intubated and then loaded onto a gurney and whisked off to the hospital with sirens blaring.
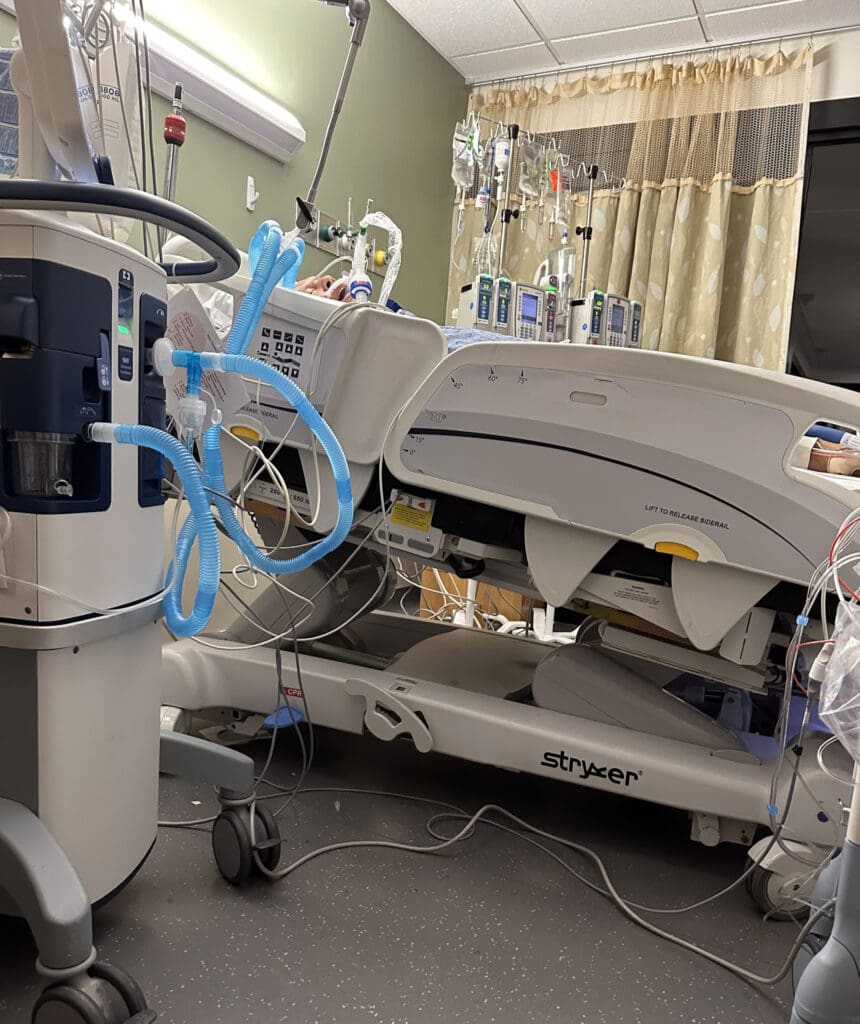
When a patient is actively dying, they no longer allow you to ride in the ambulance. This was a small mercy, as Steve continued to code multiple times on his way to Banner Boswell Hospital, just nine minutes away. Within thirty minutes of the initial attack, he was in the hospital Cath Lab. One of the best cardiologists at Boswell, Dr. Pakula, happened to be walking out when Steve was wheeled in. They grabbed him, and within forty-five minutes, a stent was in place, along with a balloon pump to help his heart function. As they battled to stabilize his failing heart, he continued to code multiple times during the procedure. Afterward, he was placed on full life support, with a balloon pumping his heart and a ventilator for his breathing.
After reviewing all his medical records, we now know he coded twenty-three times during the first hour. Steve is a miracle and became somewhat legendary during his stay at the hospital. CPR is not easy, but because he died in my arms, he was only without oxygen for about thirty seconds. That made all the difference.

His survival is nothing short of miraculous, a testament to the swift and skilled response of the heroic medical team. Now, as he recovers, I reflect on the profound gratitude we owe to all who fought for his life. This ordeal has underscored the vital importance of CPR training—a skill that proved crucial in those critical minutes.
The survival rate of a widowmaker heart attack is about 6-10% when it doesn’t occur in the hospital with a cardiologist standing by to intervene. We are so grateful for the incredible fire department and medical staff that refused to give up. Because of their heroic efforts, I can share this journey in hope that it will help others recognize the signs of a heart attack and know what to do.
Thank you for being part of our journey. I encourage everyone to learn CPR; it truly can make the difference between life and death. For those interested, the American Heart Association offers classes nationwide. This experience has not only been a testament to Steve’s strength but also to the power of community and knowledge in facing life’s most unexpected challenges.
exploring:
Leave a comment